-
ALLERGY IQ
Allergies and Health -

Children & Inhalant Allergies Allergies are a chronic disorder that starts early in life. It is one of the most common health conditions that affects one out of three children in the U.S. -

Oral Allergy Syndrome is Not Food Allergy Oral allergy syndrome (OAS) is often confused with food allergies but is not the same thing and is more common than people realize. -

Allergies & Poor Sleep Sleep is a huge factor in health and wellbeing. If your quality of sleep is affected by allergies, know that there are solutions. -

Hay Fever (Allergic Rhinitis) Unlike the common cold, hay fever is not caused by a virus. Instead, it’s caused by an allergic response to indoor/outdoor allergens like pollens, mold, mites.
-

How Allergies and Asthma are Related People who suffer from allergies can develop asthma and those with asthma can suffer from allergies. Both conditions are closely related. -

Allergy Load Find out why chronic allergic disease progresses with age, learn about Total Allergy Load, stressors, and why you don't want to delay allergy treatment.
Treating Allergies -

Managing Your Allergies Allergies are a serious burden on your immune system, not just runny nose, sneezing, and itchy eyes. Learn how to safely treat allergies for full-body health. -

Testing For Allergies: Is It Necessary? Allergy testing is a necessary step in treating symptoms of allergic rhinitis. Skin and blood tests can find the source and ideal treatment for your symptoms. -

Nasal Steroid Sprays Due to their high efficacy and safety, nasal steroid sprays are considered the first line of treatment for allergic rhinitis and other nasal conditions. -

Nasal Obstruction, Inhalant Allergies, and Turbinate Reduction Inhalant allergies can cause nasal obstruction and enlarged turbinates. Learn about the causes and treatment options for your chronic congestion.
-
- ALLERGY EXPLORER
- ALLERGY QUIZ
- SEARCH
- ACCOUNT
ORAL ALLERGY SYNDROME IS NOT FOOD ALLERGY
Oral allergy syndrome (OAS), an allergic reaction to proteins in fruits or vegetables, affects many people who suffer from seasonal pollen allergies. Over the past years, OAS medical professionals and allergy sufferers have given more focus to this interesting condition.
What is OAS?
Some fresh fruits and vegetables contain proteins similar to those found in pollen. This is why OAS is also known as Pollen-Food Allergy Syndrome (PFAS).
Most allergists define OAS as a cross-reactivity reaction, where a person develops an allergic reaction after eating certain raw fruits or vegetables. This reaction includes visible symptoms like itching and redness of the mouth, lips, and throat.
In simpler terms, the person is not allergic to the food but rather to the proteins inside the food that are similar to pollen proteins. Their immune systems cannot differentiate between pollen and food proteins. Because of that, the immune system mistakenly causes an allergic reaction as if that person was exposed to the pollen itself.
Unlike seasonal allergies, OAS can occur at any time of year when a trigger food is eaten. However, the symptoms are often worse during allergy season.
Why is it called “Oral” allergy syndrome?
The majority of OAS symptoms – if not all – are focused in the mouth region. These symptoms include redness, mild swelling, and itching of the lips, face, tongue, cheeks, or throat. OAS can cause more severe reactions like chest tightness, difficulty breathing, and loss of consciousness in extreme cases.
How is OAS different from food allergy?
Although OAS sounds like a food allergy, it is quite different. A food allergy is a sensitivity to the proteins in a specific type of food, most commonly milk, eggs, peanuts, tree nuts, fish, shellfish, wheat, and soy. However, a person with an OAS has no food allergy but still develops mild allergic reactions in their mouth after eating certain foods.
Prick and blood allergy tests are used to determine if a person is allergic to a particular substance. People with OAS test negative for food allergies on these tests. That OAS allergic reaction is not associated with the food itself but with other proteins in the food that resemble the proteins in a pollen to which they have a sensitivity.
Unlike food allergies, OAS symptoms are usually mild, limited to redness, itching, and slight swelling of the mouth's tissues. Very few people develop severe allergic reactions such as tightness of the throat or chest, hives, difficulty breathing, vomiting, or loss of consciousness.
Another key difference is the timeframe of the development of the symptoms. Symptoms of food allergies often appear approximately 2 hours after consumption, and in some cases, occur up to 6 hours later. With OAS, symptoms may start to appear as soon as 5 to 20 minutes after consuming the food.
There is also a connection between mold and food allergies. While a person may not be allergic to a specific food, they may be allergic to mold that accumulates on the surface of the food. A mold allergy could cause reactions similar to the OAS response. These should not be confused with symptoms of OAS, which tend to be concentrated in the mouth and face.
What to be on the lookout for?
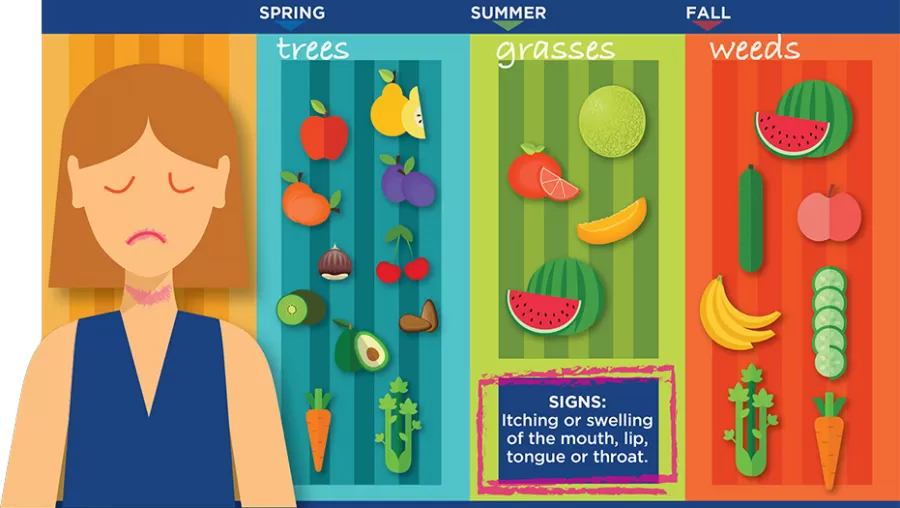
Each specific pollen allergen is associated with fruits and vegetables that have similar proteins. Examples include:
1.
Birch tree pollen allergy: pitted fruits (apples, peaches, pears, and apricots) as well as carrots, celery, and parsley
2.
Timothy and orchard grass allergy: oranges, tomatoes, and white potatoes
3.
Ragweed allergy: melons (cantaloupes, watermelon, and honeydew) as well as zucchini
4.
Mugwort allergy: vegetables (bell peppers, broccoli, and cabbage) as well as spices (black pepper, caraway, and aniseed)
Parents might notice signs of picky eating in their children, but fussy appetites could be because of an allergic reaction in the child's mouth. If this happens, ask the child if their mouth or throat is itching or feels swollen. A child may not even be aware that they are experiencing these symptoms and needs an adult's help to identify them.
Heat destroys the proteins that cause these allergic reactions. In the case of children’s OAS, if the child accepts the food in a cooked or canned form, it could be further evidence of an underlying allergy.
For adults, the symptoms are the same - itching, swelling, and redness in the mouth, throat, and face. If you experience these symptoms, especially after eating known trigger foods, you may have OAS.
How to deal with OAS?
When addressing OAS, the most important thing is first to make sure there is no actual food allergy present. Food allergies can be life-threatening and need to be treated immediately. The only way to determine if the reaction is from a food allergy is through a skin prick or blood test.
If testing in either form is negative, the fruit or vegetable that caused OAS can likely be safely consumed. However, neutralizing the proteins that can cause OAS can also reduce the risk. Cooking the food destroys the allergenic proteins, while peeling fruit or vegetables may remove the most concentrated proteins from the skin.
OAS symptoms are treated the same as inhalant allergies. For example, over-the-counter antihistamines can reduce reactions in some cases.
But the most effective way to eliminate OAS symptoms is through immunotherapy. Your allergist can give you an intradermal allergy screening test to determine your sensitivity, then explain treatment options like immunotherapy shots or drops. Immunotherapy is a long-term solution to allergies that can help you live a happy, symptom-free life.
